IVF, Test Tube Baby & Advanced Laproscopic Center
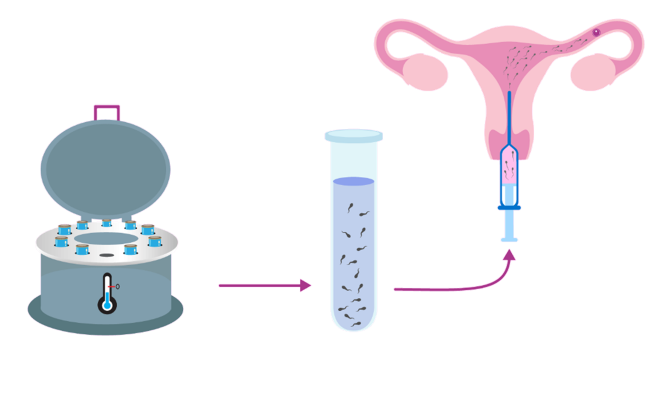
IUI – Intrauterine Insemination
In this procedure, husband semen/donor semen is washed to remove the debris, pus cells & bacteria & is placed inside the uterine cavity by a special catheter (Insemination cannula).
The process is painless, easy & an OPD procedure. It requires no sedation or anesthesia.
The ovaries are gently stimulated with oral tablets either alone or with low dose hormone injections followed by ultrasound monitoring until the follicles are mature when HCG trigger is given. The aim is to stimulate the release of one or two eggs only. Insemination is performed around the time of ovulation.
It increases the chances of pregnancy as the semen quality is improved by washing, the quality of egg is improved by medicine & the timing of insemination is set with the ovulation.
The success rate with this procedure is in the range of 10 – 15 % and 3 – 6 cycles are generally advocated before proceeding to higher ART procedures
Factors influencing outcome of IUI:
- Age and duration of infertility
- Semen quality
- Indication of IUI
- Ovarian stimulation protocol
- Semen preparation
- Timing of IUI
- Technique of IUI
- Number of inseminations
Indications of IUI:
- Anovulatory infertility
- Unexplained infertility
- Azoospermia (nil sperms)
- Cervical factor
- Endometriosis
- Immunological
- Male factor

IVF technique is now mainly used in the following cases:
- Females with one or both fallopian tubes blocked
- Borderline male sperm count
- Endometriosis
- Unexplained infertility cases
- Couples who have failed the traditional treatments like timed intercourse, follicular monitoring, IUI etc.
- Couples who require donor egg IVF
Now a day’s age and attaining menopause are not a constraint to experience motherhood. IVF (In Vitro Fertilization) has proved to be a boon to all those couples who’ve only dreamt of becoming parents but could never see their dream coming true due to insurmountable reasons.
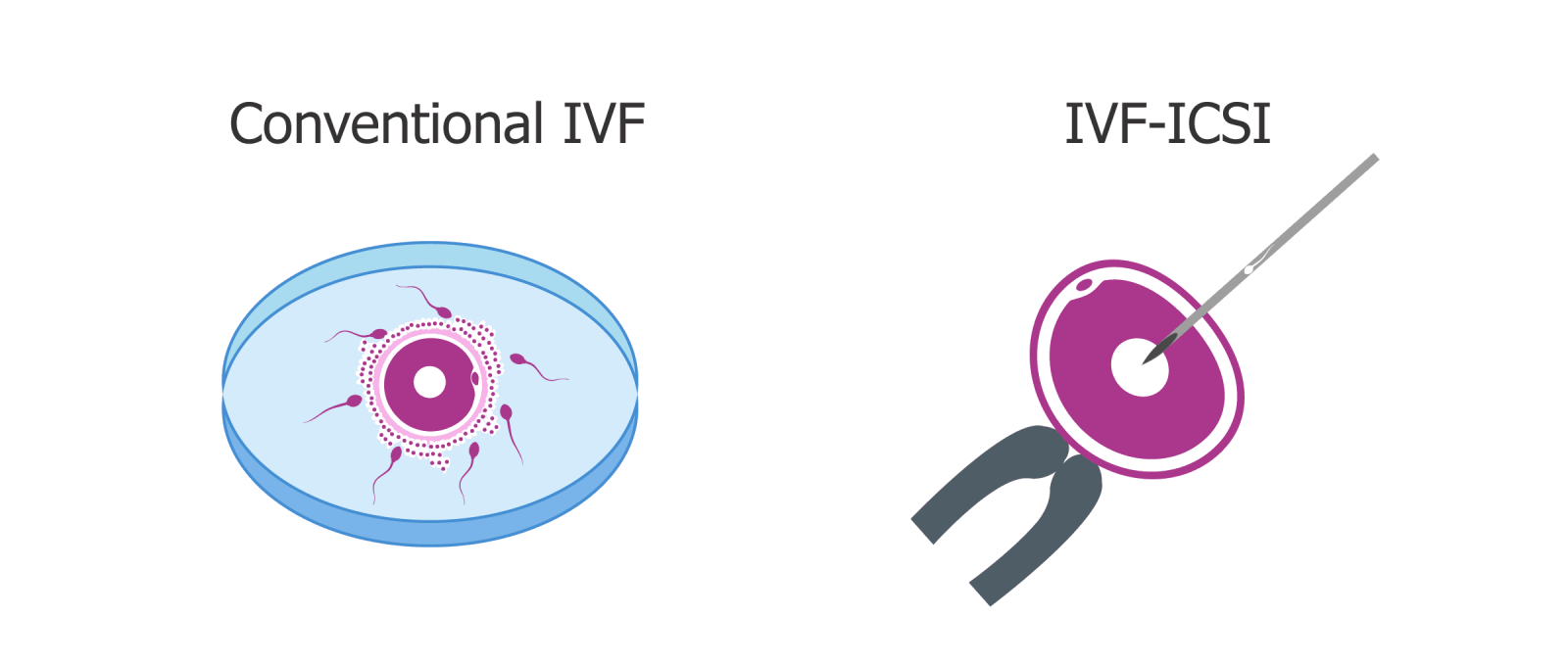
IVF – In Vitro Fertilization
IVF literally means ‘fertilization outside the body,’ more simply explained as ‘test tube baby’. In the IVF process, eggs are removed from the ovaries of the female and at the same time sperms are collected from the male partner. The eggs and sperms are made to fertilize in the laboratory and the fertilized egg (embryo) is then implanted in the woman’s womb to make her conceive.
Steps involved in IVF/ICSI:
- Comprehensive evaluation of both partners
- We formulate the treatment strategy, explain the procedure, prognosis, costs, risks, benefits and offer counseling support.
- If IVF-ICSI treatment is recommended, we carry out the following sequence: hormonal injections for controlled stimulation.
- Ultrasound monitoring to check the follicular growth.
- The eggs are collected under anesthesia (one day at the clinic) and the husband’s sperm is collected.
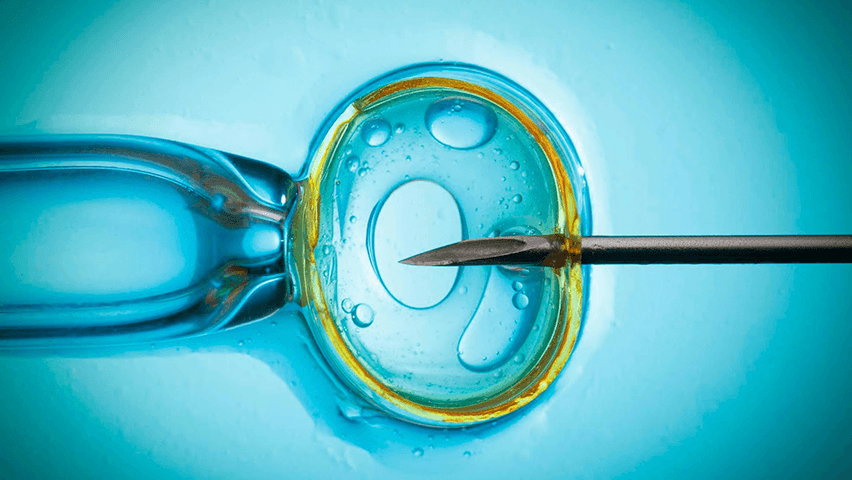
- Fertilization. In a state-of-the-art, dust-free lab, the man’s sperm is injected into the egg by skilled embryologists.
- The best embryos are selected and transferred on the 2nd, 3rd or 5th day after egg were collected.
- 15 days later, a pregnancy test is done.
NOTE: Other good quality embryos can be frozen on request for future cycles if necessary. This prevents the need to undergo step 1 to 6 again.
ICSI – Intracytoplasmic Sperm Injection
This technique has been the greatest boon to male factor infertility which does not respond to conventional management, i.e. men with low sperm count and motility. As with IVF, the oocytes are aspirated. On a special microscope with a micromanipulator, a single sperm is picked up in a fine microneedle and injected manually into the oocyte. Embryos are transferred after 48 to 72 hours.
For azoospermic men with an obstructive pathology (e.g.: Congenital absence of vas deferens) sperm can be aspirated directly from the epididymis (PESA) and used for ICSI. In addition, for azoospermic men with a non-obstructive pathology, sperm can be retrieved directly from the testis (TESE) and used for ICSI.

Indications for ICSI:
- Sperm completely absent in semen (Azoospermia)
- Sperm present in poor concentration
- Poor Sperm motility
- Poor Sperm Morphology
- History of fertilization failure with conventional IVF
- Sperm retrieved by surgical techniques (TESE/ PESA)
- If pre-implantation genetic diagnosis (PGD) is being used to screen embryos for some specific genetic disorder
Semen Cryopreservation is done for the following reasons:
- To develop semen bank for donation purpose
- To use it during the treatment if the male partner is unable to ejaculate on the stipulated day before undergoing vasectomy
- Prior to cancer treatment which might adversely affect fertility
- Surgically Retrieved sperm from epididymis (PESA) or testes (TESA)
Embryos Cryopreservation is done during treatments like IVF, ICSI the best embryos are selected and transferred during the first cycle. If any good quality embryos are left, they are frozen for future use.

Cryopreservation
This is a technique in which sperms, eggs and embryos are frozen at a sub-zero temperature to preserve them for future when the need arises. The types of Cryopreservation available are:
- Semen Cryopreservation
- Embryos Cryopreservation
3rd Party Reproduction with Donor Programme
Semen Donation: Semen from a donor obtained through a semen bank is required in the following cases:
- Male partner has azoospermia (absent sperm in semen) or his sperm are of low-quality
- Male partner has ejaculatory dysfunction
- Female partner is RH negative and severely RH iso immunized and male partner is RH positive.
- Male partner has a significant genetic defect or the couple previously had a child affected by a condition for which carrier status cannot be determined.
- Male partner has a sexually transmissible infection that cannot be eradicated.
Egg Donation: When female partner is unable to produce eggs or her eggs can’t be used due to various reasons like:
- Menopause/ Advanced reproductive age
- Premature ovarian failure/ hypogonadotropic hypogonadism
- Diminished ovarian reserve
- Women who are known to be affected by or known to be the carrier of a significant genetic defect or who have a family history of a condition for which carrier status cannot be determined
Women with poor egg and/or embryo quality or multiple previous failed attempts to conceive via ART
The donor eggs are fertilized and implanted in the womb of the female partner. The ICMR guidelines for IVF clinics in India permits egg donation and the use of egg donors for this purpose. Our clinic maintains the highest standards for selection of egg donors, screening for disease, repeat checks for sexually transmitted diseases such as HIV, Hepatitis B, C and syphilis and other checks as requested by couples
Embryo Donation: When both the male partner and the female partners are infertile, they opt for embryo donation. In this, the embryo is developed by fusing the sperm and eggs of donors and the embryo is implanted in the uterus of female partner. The couples who are donating the sperm and the eggs undergo a series of tests to rule out any medical ailment and ensure good quality of sperm & eggs.

Surrogacy
Gestational surrogacy is a treatment option available to women with certain clearly defined medical problems, usually an absent uterus, to help them have their own genetic children. IVF allows the creation of embryos from the gametes of the commissioning couple and subsequent transfer of these embryos to the uterus of a surrogate host.
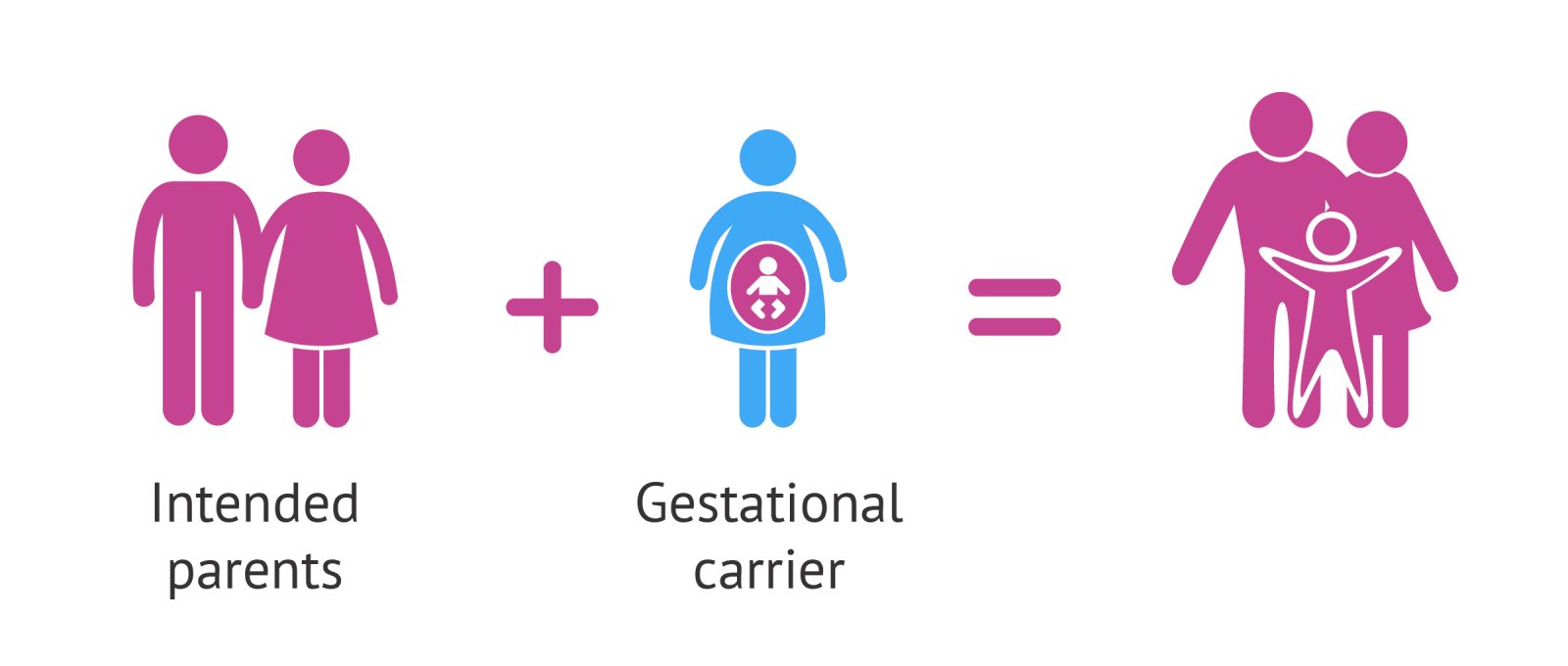
The indications for treatment include:
- Not having a uterus as a result of a hysterectomy or being born without a functional uterus
- Significant uterine abnormalities, including uterine scarring (Asherman’s Syndrome) and inability to develop a thick, supportive uterine lining
- Significant medical conditions that make carrying a pregnancy risky for a woman’s health (such as hypertension)
- Recurrent miscarriages
- Altruistic surrogacy is done for married Indian couples.
